Can Limited Scleroderma Become Systemic? What You Need To Know
Many folks living with limited scleroderma often wonder about its future path. It's a really common question, you know, because the way this condition acts can be a bit of a mystery sometimes. People want to get a good sense of what might happen down the road, and that's totally fair. Knowing more helps you feel a bit more in control, and that's a good thing.
Limited scleroderma, sometimes called limited cutaneous systemic sclerosis, typically shows up in specific body areas. It mostly affects the skin on your hands, your forearms, your feet, and your face, you see. For many, it can stay put in these spots for quite a long time, which is a bit of a relief in some ways. Yet, the thought of it changing, or moving to other parts of the body, can be pretty concerning, and that's a very real feeling for people.
This article will look into that very question: Can limited scleroderma actually become systemic? We'll talk about what that means, and what to keep an eye on. We'll also cover some things you can do to manage your health, and, you know, just generally stay informed about your condition. It's about getting clear information, and that's what we aim to provide here.
Table of Contents
- What Scleroderma Is All About
- The Question of Progression
- Why This Matters for Your Health
- Staying Informed and Taking Action
- Frequently Asked Questions
What Scleroderma Is All About
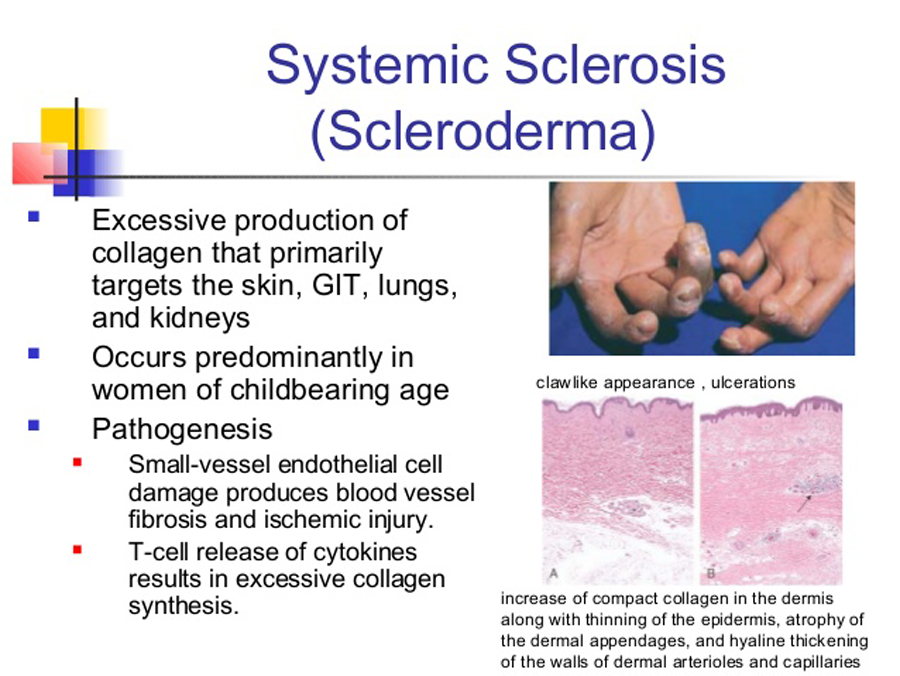
Scleroderma is a long-term condition that affects your connective tissues, you know, the stuff that holds your body together. It's an autoimmune disease, which means your body's defense system mistakenly attacks its own healthy tissues. This causes too much collagen to build up, and that's what leads to the hardening and tightening we see, especially in the skin, so it's a bit complicated.
This condition can show up in different ways, and, you know, it acts differently for each person. Some people might have mild symptoms, while others could experience more widespread effects. It's a very individual thing, so what one person goes through might not be what another person experiences at all. That's why understanding your specific type is really important.
When we talk about scleroderma, we are usually thinking about two main types. There is localized scleroderma, and then there is systemic scleroderma. Localized forms tend to be milder and usually affect only the skin, or perhaps the tissues just under the skin. Systemic forms, however, are a bit more involved, and that's where the real concern often comes in.
Limited Versus Systemic Forms
Limited scleroderma, also known as limited cutaneous systemic sclerosis, is one of the systemic types, actually. It usually starts with skin changes on the hands and feet, and maybe the face, too. People with this type often have Raynaud's phenomenon for many years before other symptoms show up. That's where your fingers and toes get really cold and change color in response to cold or stress, you know, it's a very distinct symptom.
This form can also involve certain internal organs, but typically, it does so later and more slowly than the diffuse systemic type. For instance, people might develop issues with their esophagus, or perhaps, you know, a specific kind of lung problem called pulmonary hypertension. These internal issues can be serious, but they tend to progress at a slower pace, which is often a small comfort.
Systemic scleroderma, or systemic sclerosis, is the broader term. It includes both limited and diffuse types. Diffuse cutaneous systemic sclerosis is the other main type, and it tends to affect larger areas of skin, including the trunk and upper arms and legs. It also often involves internal organs much earlier and more rapidly, which is a bit more concerning for people. That's why the distinction between limited and diffuse is quite important.
The key difference, then, is the extent of skin involvement and the speed at which internal organs might be affected. Limited scleroderma, you see, has a more restricted pattern of skin changes and a slower progression of internal issues, typically. Diffuse scleroderma, on the other hand, just affects more of the body, and it does so more quickly, which is a bit of a challenge for those living with it.
The Question of Progression
So, the big question is, can limited scleroderma actually become systemic? Well, the answer is a bit nuanced, you know. Limited scleroderma *is* a form of systemic scleroderma already. The "systemic" part means it has the potential to affect internal organs, not just the skin. The "limited" part just refers to the extent of the skin hardening, which is usually restricted to certain areas, you see.
What people usually mean when they ask if it can "become systemic" is whether it can change from the limited skin form to the more widespread, diffuse skin form, or if new, more severe internal organ issues will develop. It's a very fair point to wonder about, as the idea of things getting worse is naturally concerning. The way it works is that the internal organ involvement, while possible from the start, tends to show up later with limited scleroderma.
It's not that limited scleroderma transforms into diffuse scleroderma, per se. They are considered different subsets from the beginning, usually. However, someone with limited scleroderma can certainly develop internal organ complications over time. These complications are part of the systemic nature of the disease, even if the skin changes remain limited. So, it's more about the progression of internal issues than a change in the type of skin involvement, in a way.
The disease can progress, yes, but it often does so slowly for those with the limited form. This slow pace is one of the defining features of limited scleroderma, actually. It gives people more time to, you know, adjust and manage symptoms as they appear. Still, staying aware of potential changes is very important for long-term health, and that's something doctors really emphasize.
Understanding Systemic Involvement
When we talk about systemic involvement in limited scleroderma, we're talking about the disease affecting organs beyond the skin. This could mean problems with your digestive tract, like difficulty swallowing because of changes in your esophagus. It's a common issue, and it can be pretty uncomfortable, you know, making eating a bit of a chore sometimes.
Another area of concern is the lungs. Some people might develop pulmonary hypertension, which is high blood pressure in the arteries of the lungs. This can make you feel short of breath, and it can be quite serious if not caught early. It's a very important thing to monitor, and doctors often do regular checks for it, you know, just to be safe.
The kidneys can also be affected, though this is less common in limited scleroderma compared to the diffuse type. Kidney problems can be very serious and need quick attention. Heart issues, like problems with the heart muscle or its electrical system, can also occur, though they are also less frequent. So, while it's "limited" in skin, it's still systemic in its potential reach, which is a bit confusing for some.
It's important to remember that not everyone with limited scleroderma will develop these severe internal problems. Many people live with the condition for years with only mild symptoms, or with manageable internal issues. The possibility is there, though, and that's why regular check-ups and monitoring are so important. You just want to catch anything early, you know, if it does start to show up.
Early Signs to Watch For
Knowing what to look for can make a real difference, you know, in managing limited scleroderma. One of the earliest signs of potential internal involvement, beyond Raynaud's, might be changes in your digestive system. This could be things like heartburn that just won't go away, or trouble swallowing food. It's not just a minor annoyance; it could be a sign, so pay attention to it.
Shortness of breath, especially when you're doing something active, or even when you're resting, is another important symptom to notice. This could point to lung involvement, like pulmonary hypertension. If you find yourself getting winded easily, or, you know, just feeling like you can't catch your breath, it's definitely something to bring up with your doctor, and that's a very serious symptom.
Swelling in your legs or feet, or unexplained weight loss, could also be signs that something else is going on. Changes in how much you're peeing, or, you know, really high blood pressure readings, might suggest kidney involvement. These are less common with limited scleroderma, but they are still things to be aware of, just in case. It's all about listening to your body, in a way.
Any new or worsening symptom, even if it seems small, should be discussed with your healthcare provider. Your doctor can run tests to see what's happening inside. Early detection of internal organ issues can lead to better outcomes, you see, because treatment can start sooner. It's about being proactive with your health, and that's a good approach to take.
Why This Matters for Your Health
Understanding the potential for progression in limited scleroderma is really important for your health. It helps you and your doctor stay ahead of things, you know. If you know what to watch for, you can bring up concerns early, and that means getting help sooner. This proactive approach can make a big difference in how the disease affects your life, actually.
It means you'll be more likely to get the right tests at the right time. For example, your doctor might suggest regular lung function tests or heart screenings, just to keep an eye on things. These tests can spot problems before they become really serious. So, it's about prevention and early action, which is always better for long-term health, you see.
Also, knowing about potential progression helps you prepare mentally. It's a lot to take in, but having information can reduce some of the worry. You can work with your healthcare team to create a personal health plan that addresses your specific needs. This plan might change over time, and that's okay, because your health needs might change, too. It's a journey, in a way.
Getting a Diagnosis
If you suspect you have scleroderma, or if your limited scleroderma symptoms seem to be changing, getting a clear diagnosis is the first step. This usually involves a physical exam where your doctor checks your skin and other symptoms. They will ask a lot of questions about your medical history, and, you know, your family's health history too. It's all part of putting the puzzle together.
Blood tests are often done to look for specific antibodies that are common in scleroderma. For example, the anti-centromere antibody is often found in people with limited scleroderma. These tests help confirm the diagnosis and also help classify the type of scleroderma you have. It's a very important piece of information, and it helps guide treatment decisions.
Your doctor might also order imaging tests, like X-rays or CT scans, to check your lungs or other internal organs. Heart tests, like an echocardiogram, might also be part of the process. These tests help paint a full picture of how the disease is affecting your body. It's about getting all the facts, so you can make informed decisions about your care, you know.
Sometimes, a skin biopsy might be done, where a small piece of skin is taken and looked at under a microscope. This can help confirm the presence of too much collagen. Getting a diagnosis can take some time, and it can be a bit frustrating, but it's a really important step towards getting the right care. You want to be sure about what you're dealing with, actually.
Managing Your Condition
Managing limited scleroderma, especially if it shows signs of progression, involves a team approach. You'll likely work with a rheumatologist, who specializes in these kinds of conditions. You might also see other specialists, like a lung doctor or a heart doctor, depending on which organs are affected. It's about having the right people on your side, you see.
Treatment usually focuses on managing symptoms and preventing further organ damage. For Raynaud's, you might use medicines that help open up your blood vessels, or, you know, just focus on keeping your hands and feet warm. For digestive issues, there are medicines to help with heartburn or improve swallowing. It's about making daily life more comfortable, in a way.
For more serious internal issues, like pulmonary hypertension, there are specific medicines that can help lower blood pressure in the lungs. These treatments can be really effective in slowing down the disease's progression and improving your quality of life. It's about finding what works best for your body, and that can take some trial and error, you know.
Physical therapy and occupational therapy can also be very helpful. They can help you keep your joints flexible and manage any skin tightening. Lifestyle adjustments, like regular, gentle exercise and a healthy diet, can also play a big role in overall well-being. It's about taking care of yourself in every way you can, actually.
Staying Informed and Taking Action
Staying informed about limited scleroderma, and its potential to involve more of your body, is truly powerful. It helps you advocate for yourself and work closely with your medical team. Knowing the signs to watch for, and, you know, what questions to ask, means you are an active participant in your own health journey. That's a very good thing for anyone dealing with a long-term condition.
Regular check-ups are absolutely key. Even if you feel well, these appointments allow your doctor to monitor your condition and catch any changes early. They can run routine tests that might spot issues before you even feel symptoms. It's a bit like, you know, doing regular maintenance on something important; you want to keep it running smoothly, actually.
Connecting with others who have scleroderma can also be a huge help. Support groups, whether online or in person, provide a space to share experiences and learn from others. You can find out more about scleroderma from reputable sources like the Scleroderma Foundation, which offers a lot of helpful resources. It's about not feeling alone, and that's really important for mental well-being, too.
Remember, while limited scleroderma is already a systemic condition, understanding its potential progression means you can take proactive steps. This includes knowing what symptoms to report and making sure you get regular screenings. Learn more about our main page on our site, and also check out this page living with scleroderma for more support. Being prepared and well-informed helps you live your best life, you know, even with this condition.
Frequently Asked Questions
People often have many questions about limited scleroderma and its effects. Here are some common ones that come up, you know, just to help clarify things a bit more.
What is the difference between limited and systemic scleroderma?
Limited scleroderma is actually a type of systemic scleroderma. The main difference is the amount of skin affected, you see. In limited scleroderma, skin hardening is mostly on the hands, feet, forearms, and face. Systemic scleroderma is the broader term, and it includes both limited and diffuse types. Diffuse systemic scleroderma affects more skin on the body, like the trunk, and can involve internal organs earlier and more quickly. So, limited is just one specific way systemic scleroderma shows up, actually.
How quickly does limited scleroderma progress?
Limited scleroderma generally progresses very slowly, you know, over many years. It's common for people to have Raynaud's phenomenon for a long time before other symptoms appear. While internal organ involvement can happen, it tends to develop later in the disease course and at a more gradual pace compared to the diffuse form. The progression speed can vary a lot from person to person, but it's typically a slow process, which is often a bit of a relief for those affected.
What are the early signs of systemic scleroderma?
Early signs of systemic scleroderma can include Raynaud's phenomenon, which is often the first symptom for many. Skin changes like swelling, thickening, or tightening, especially on the fingers and hands, are also common. Other early signs might involve joint pain, or, you know, digestive issues like heartburn or difficulty swallowing. If you notice these things, it's a good idea to talk to your doctor, just to get it checked out, you see.
Scleroderma - Myositis Support and Understanding
Systemic Scleroderma Hands
.jpg)
Systemic sclerosis. - ppt download