What Is The History Of Scleroderma? Uncovering Its Centuries-Old Story
Have you ever wondered about the journey of medical discovery, particularly for conditions that seem so complex today? Well, if you have, then you might find the story of scleroderma's past quite compelling. This condition, which affects the body's connective tissues, really has a long and somewhat winding history of being understood, and it spans many centuries, you know. It's a tale of keen observation and slow, steady learning.
It's fascinating, isn't it, to consider how people in earlier times grappled with health issues that we now have names for and a bit more insight into. The history of scleroderma, in a way, shows us how medical knowledge builds up, little by little, over generations. People observed symptoms, tried to make sense of what they saw, and then, you know, they tried to find ways to help.
So, we're going to take a look at this history, tracing the path from early, vague descriptions to the much clearer picture we have today. This journey of discovery helps us appreciate just how far medical science has come, and it also, quite frankly, gives us a better sense of the condition itself. It's a pretty interesting story, actually, of how a mysterious illness slowly became something recognized and studied.
It's important to mention, as a matter of fact, that the specific text you provided about Google account activity and history deletion is not relevant to the medical history of scleroderma. Therefore, it cannot be used as a source for the factual information within this article. The historical details presented here come from general medical knowledge and historical records concerning the condition.
Table of Contents
- Early Glimpses and Ancient Observations
- The Renaissance and First Detailed Accounts
- The 19th Century: Naming and Defining
- The 20th Century: Deepening Understanding
- The Modern Era: Genetics and Targeted Therapies
- Frequently Asked Questions About Scleroderma History
Early Glimpses and Ancient Observations
When we look way back in time, it's pretty hard to pinpoint the very first mention of something that clearly matches scleroderma. That's because, you know, ancient medical writings often described symptoms without giving them specific names or understanding the underlying causes. People just saw what was happening to the body. So, early writings from places like ancient Egypt or Greece might have talked about skin changes or hardening, but they didn't really connect it to a distinct illness like we do today. It was more about observing general physical signs, actually.
For example, some scholars suggest that certain descriptions of skin conditions in old texts, like those from Hippocrates, could potentially, just potentially, refer to something resembling scleroderma. These were observations of skin becoming stiff or tight, or maybe losing its usual feel. But, honestly, these were very broad descriptions, and they didn't have the detailed clinical picture we now associate with this specific condition. They were just, you know, noting unusual skin. There wasn't a specific diagnosis for it back then, obviously.
It's a bit like looking for a needle in a haystack, trying to find a perfect match for scleroderma in those very old records. The medical language was different, and the way illnesses were categorized was, quite frankly, very basic. So, while the symptoms might have been present in people, the formal recognition and description of scleroderma as a unique disease had to wait for later periods, when medical observation became a little more refined, and, you know, more systematic.
The Renaissance and First Detailed Accounts
The true story of scleroderma's recognition really starts to take shape during the Renaissance, that period of great rebirth in art, science, and, you know, medicine. This was a time when doctors began to look more closely at the human body, conducting dissections and making more careful, detailed notes about what they observed in their patients. They were starting to move away from older theories and really focusing on what they could see and feel, which was a pretty big step.
One of the earliest, and perhaps the most cited, detailed accounts of what sounds very much like scleroderma comes from a doctor named Girolamo Mercuriale. This was in 1573, and he was an Italian physician. He described a case of a woman whose skin had become hardened and tightened, making it difficult for her to move her body. He called it a "sclerosi," which, you know, means hardening. This was a pretty significant moment, as it was a much more specific description than anything seen before, and it really pointed to a distinct set of symptoms, actually.
Mercuriale's description, in a way, laid some groundwork. It wasn't just a general observation; it was a clinical report, noting the progression and the impact on the person's daily life. This was a big change from the vague mentions of earlier times. It showed a growing interest in classifying diseases based on their unique characteristics, and, you know, it helped future doctors recognize similar cases when they encountered them. It was, arguably, a turning point in how this condition was perceived.
Carlo Curzio and the 18th Century
Moving into the 18th century, the understanding of scleroderma got another important push, thanks to a doctor named Carlo Curzio. In 1753, he published a very detailed case report of a young woman with skin that was, you know, remarkably hardened and tight. She couldn't open her mouth fully, and her movements were quite restricted because of this skin condition. Curzio's description was incredibly thorough, really painting a clear picture of the symptoms. He even noted the internal effects, which was, for his time, very advanced thinking, actually.
Curzio's work was pretty remarkable because he didn't just describe the outward appearance; he tried to understand the deeper aspects of the illness. He recognized that this wasn't just a surface problem; it was something that affected the body in a more profound way. His detailed observations helped other physicians grasp the true nature of the condition, and, you know, it helped separate it from other skin ailments that might have looked similar on the surface. It was a very important contribution, in some respects.
His report, you know, served as a key reference for later doctors who were trying to make sense of this unusual hardening of the skin. It showed that the condition was not just a curiosity but a serious illness with widespread effects. This kind of careful documentation was vital for the slow but steady progress of medical knowledge, and it helped build a foundation for future studies. It was, quite literally, a step forward in recognizing a complex disease.
The 19th Century: Naming and Defining
The 19th century was a really crucial period for scleroderma. This was when the condition finally got its widely accepted name, and doctors began to differentiate it more clearly from other illnesses. It was a time of more systematic medical classification, where physicians were trying to put diseases into neat categories based on their specific features. This was, you know, a big step towards modern medicine, where precise diagnoses are so important, obviously.
Before this time, people might have just called it "hard skin" or something similar. But as more cases were observed and documented, it became clear that this was a distinct condition that needed its own identity. Doctors were, in a way, trying to organize the vast amount of medical information they were gathering. So, giving it a proper name was a really important part of that process, and it helped everyone talk about the same thing, you know, with clarity.
This period also saw more doctors publishing their findings, sharing their observations of patients with similar symptoms. This collaborative effort, where information was exchanged across different regions and countries, really helped build a more comprehensive understanding of the disease. It showed that this condition wasn't just an isolated occurrence but something that affected people broadly. It was, basically, a time of collective learning and naming.
Alibert and the Term "Scleroderma"
The term "scleroderma" itself, which means "hard skin" in Greek, was coined by a French dermatologist named Jean-Louis Alibert. This happened in 1817, and it was a pretty significant moment. Alibert used this term to describe a condition where the skin became very tough and rigid. His work helped solidify the name for the disease, making it easier for doctors all over the world to refer to it consistently. It was, you know, a simple but powerful act of naming, really.
Alibert's contribution was more than just a name, though. He provided detailed descriptions of patients, helping to distinguish scleroderma from other skin conditions that might have had some similar features. He was, in a way, creating a clear picture of the disease for others to recognize. This precision in description was really important for advancing medical knowledge, and it helped doctors to, you know, make more accurate diagnoses. It was a very important step in formalizing the condition.
His work was part of a larger movement in medicine to categorize and define diseases more precisely. Before this, diagnosis could be pretty vague. But with terms like "scleroderma," physicians could communicate more effectively about specific conditions, and that, you know, helped lead to better understanding and, eventually, better care. It was a moment where a specific illness got its true identity in the medical world, actually.
Further Differentiation and Study
After Alibert's naming, other physicians continued to study scleroderma, adding to the growing body of knowledge. In 1842, Giovanni Battista Fantonetti, an Italian physician, provided more insights into the disease. He described cases where the hardening wasn't just on the skin but also affected deeper tissues, like muscles and even internal organs. This was a pretty big realization, showing that scleroderma was, you know, a systemic condition, meaning it could affect the entire body, not just the skin. It really broadened the understanding of the illness.
This deeper understanding of scleroderma as a systemic disease was really important. It meant that doctors had to look beyond just the skin symptoms and consider how the condition might be affecting other parts of the body. This led to more comprehensive examinations and, you know, a more holistic view of the patient's health. It was a shift from just treating symptoms to trying to understand the full scope of the illness, which was, quite frankly, a big leap forward in medical thinking.
Throughout the rest of the 19th century, more and more case reports and studies emerged. Doctors began to recognize different patterns in how scleroderma presented itself, noting variations in its severity and the specific organs it affected. This period was, in a way, about filling in the details of the disease, making the picture clearer and more nuanced. It was a time of careful observation and, you know, building up a detailed profile of the condition, bit by bit.
The 20th Century: Deepening Understanding
The 20th century brought about a massive acceleration in medical understanding, and scleroderma was no exception. With advancements in technology, laboratory techniques, and, you know, research methods, doctors and scientists began to unravel some of the mysteries behind this complex condition. It was a period where the focus shifted from just describing symptoms to trying to understand the underlying biological processes, which was, quite literally, a game-changer for medicine.
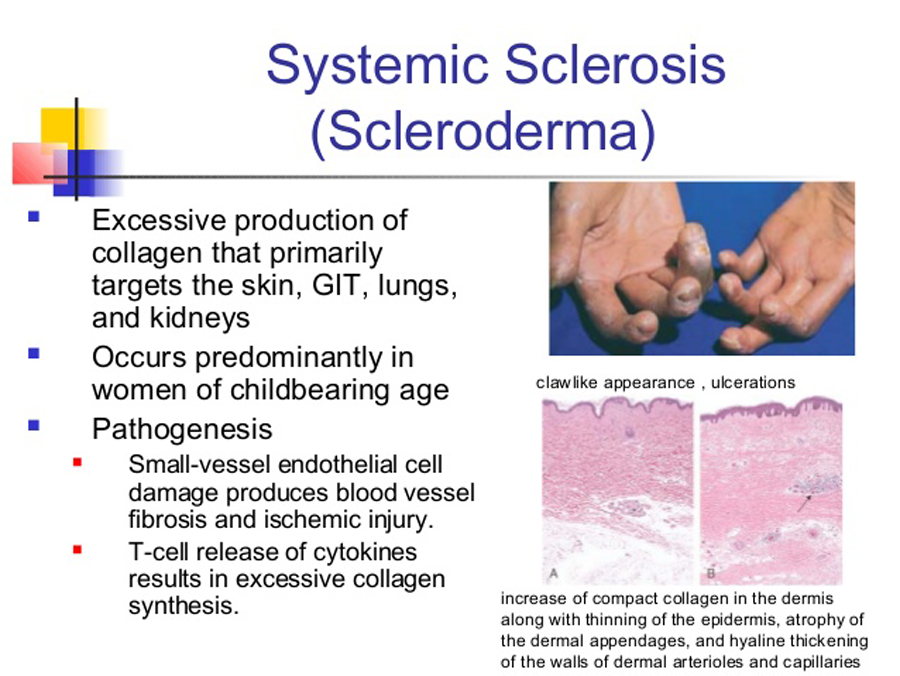
One of the biggest breakthroughs was the realization that scleroderma involves the immune system. Scientists began to discover that the body's own defense system, for some reason, starts attacking its own healthy tissues, leading to the characteristic hardening and scarring. This understanding of it being an autoimmune disease was, you know, a huge step. It opened up entirely new avenues for research and, eventually, for treatment. It helped explain why the body reacted the way it did, basically.
The development of new diagnostic tools, like specific blood tests that could detect certain antibodies, also played a vital role. These tests helped doctors confirm a diagnosis of scleroderma more accurately and even identify different forms of the disease. This meant patients could get a diagnosis sooner, and, you know, that's really important for managing a long-term condition. It was a time of really significant progress in identifying and understanding the disease at a deeper level.
Classification and Subtypes
As doctors learned more about scleroderma, it became clear that it wasn't just one single disease but rather a group of related conditions with varying degrees of severity and different patterns of organ involvement. This led to the classification of scleroderma into different subtypes. The two main forms recognized were, you know, localized scleroderma and systemic sclerosis.
Localized scleroderma, also known as morphea, primarily affects the skin, causing hardened patches. It usually doesn't involve internal organs, which is a pretty important distinction. Systemic sclerosis, on the other hand, is the form that can affect not only the skin but also, you know, internal organs like the lungs, heart, kidneys, and digestive tract. This distinction was really important for treatment planning and for giving patients a better idea of what to expect, actually.
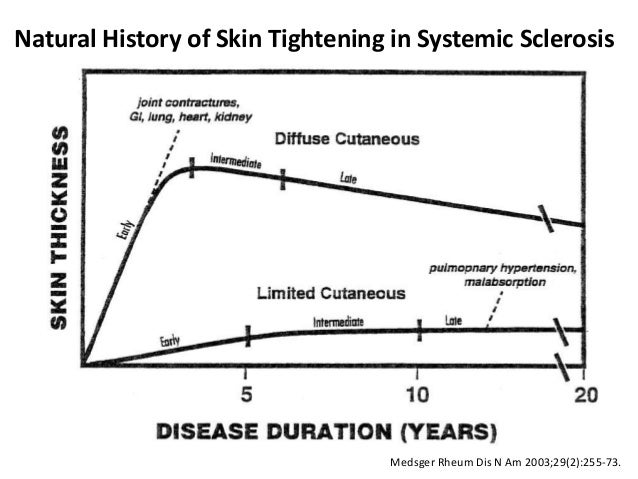
Further refinements led to the identification of even more specific subtypes within systemic sclerosis, such as limited cutaneous systemic sclerosis (CREST syndrome) and diffuse cutaneous systemic sclerosis. These classifications, you know, helped doctors predict the course of the disease more accurately and tailor treatments to the individual patient's needs. It was about bringing order to a complex set of symptoms, and, quite frankly, making it easier to manage the condition.
Early Treatment Approaches
With a better understanding of the disease, the 20th century also saw the beginning of more targeted treatment approaches for scleroderma. In earlier times, treatments were often very general and aimed at just easing symptoms, like using ointments for skin stiffness or, you know, trying to improve circulation. But as the autoimmune nature of the disease became clearer, doctors started to explore medications that could modulate the immune system.
For instance, corticosteroids, which are powerful anti-inflammatory drugs, were among the first medications used to try and control the immune response. While they weren't a cure, they could help reduce inflammation and, you know, slow down the progression of some symptoms. Other drugs that suppressed the immune system, like methotrexate, also began to be used, especially for more severe forms of the disease. These were, in a way, early attempts to get at the root cause, actually.
Beyond medications, supportive therapies became increasingly important. Physical therapy helped maintain mobility and flexibility in joints and skin. Occupational therapy helped people adapt to daily tasks as their bodies changed. These approaches, you know, focused on improving the patient's quality of life and managing the long-term effects of the disease, which was, frankly, a very compassionate approach. It was about managing a chronic condition with a combination of methods, basically.
The Modern Era: Genetics and Targeted Therapies
As we move into the 21st century, the story of scleroderma continues to unfold with even more exciting developments. The focus has really shifted towards understanding the disease at a genetic and molecular level. Scientists are using advanced techniques to look at the genes involved in scleroderma, trying to figure out why some people get the disease and others don't. This genetic research is, you know, incredibly important for finding new ways to prevent or even cure the condition.
One of the most promising areas of modern research is the development of targeted therapies. Instead of using broad-acting immune suppressants, scientists are working on drugs that specifically target the pathways involved in scleroderma's progression. For example, some new medications aim to block the excessive production of collagen, which is the protein responsible for the hardening and scarring. These treatments are, you know, designed to be more precise and have fewer side effects, which is a big benefit for patients, obviously.
There's also a growing emphasis on personalized medicine. This means tailoring treatments to each individual patient, based on their specific genetic makeup, the type of scleroderma they have, and, you know, how their disease is progressing. It's a very forward-thinking approach, aiming to provide the most effective treatment for each person. This ongoing research and the continuous development of new therapies offer a lot of hope for people living with scleroderma today. You can learn more about current research on our site, and also find additional information on this page about living with scleroderma.
Frequently Asked Questions About Scleroderma History
Here are some common questions people ask about the historical journey of scleroderma:
When was scleroderma first identified?
While vague descriptions of hardened skin might appear in very old texts, the first truly detailed and recognizable account of what we now call scleroderma was given by the Italian physician Girolamo Mercuriale in 1573. He described a woman with skin hardening, calling it "sclerosi." Later, Carlo Curzio provided another very detailed case report in 1753, further clarifying the condition. So, you know, it's a bit of a gradual identification process.
Who discovered scleroderma?
No single person "discovered" scleroderma in the way one might discover a new land. Instead, its understanding grew through the contributions of many physicians over centuries. Girolamo Mercuriale and Carlo Curzio provided early, detailed descriptions. The term "scleroderma" itself was coined by the French dermatologist Jean-Louis Alibert in 1817. So, it was, you know, a collective effort of observation and naming.
What were the early treatments for scleroderma?
In earlier times, treatments for scleroderma were pretty limited and often aimed at just easing symptoms. These might have included applying topical ointments to the skin to try and soften it, or using baths and massages to improve circulation and flexibility. As the 20th century progressed and the autoimmune nature of the disease became clearer, doctors started using medications like corticosteroids and other immune-suppressing drugs to try and manage the underlying processes. It was, you know, a gradual evolution of treatment approaches.
Skin Manifestations of Scleroderma, by Dr. Lorinda Chung MD
Scleroderma - Myositis Support and Understanding
The History of Scleroderma | Scleroderma News